 Research Article
Research Article
Low Intensity Pulsed Ultrasound [LIPUS] and Shoulder Osteoarthritis Mitigation and Functional Restoration Potential Among Older Adults with Rotator Cuff Damage Mini Review and Commentary
Ray Marks, Department of Research, Osteoarthritis Research Center, Canada.
Received Date:September 23, 2025; Published Date:October 07, 2025
Abstract
Osteoarthritis, a widespread disabling disease involving an array of destructive joint tissue abnormalities and pain is highly limiting when present at the aging shoulder. Low intensity pulsed ultrasound [LIPUS], a biophysical modality of low frequency sound waves with demonstrated utility in bone healing, articular cartilage chondrocyte cell metabolism, tendon repair and inflammation that may all impact the disease in a favourable way. This current review focuses on two questions: a) whether LIPUS can yield any clinically relevant impacts on osteoarthritis related shoulder dysfunction in cases who have damaged the rotator cuff tendons; b) whether observed data support a role for LIPUS in efforts to foster life quality safely and cost effectively in this cohort. Drawn from the peer reviewed literature, basic or preclinical studies published in the last five years are specifically reviewed. From this we conclude LIPUS can be safely applied for older adults suffering from intractable should pain. It may prove restorative as well as remediate daily functional ability.
Keywords:Articular Cartilage; Low Intensity Pulsed Ultrasound [LIPUS]; Shoulder Osteoarthritis; Rotator Cuff; Tendon; Therapy
Introduction
Osteoarthritis, a disabling joint disease is one persistently creating much suffering in later life, no matter where the older person resides [1]. Generally considered progressive, rather than readily reversible or simple to arrest, this condition whose origins remain uncertain is commonly distinguished by pathological alterations in the joint capsule and its synovial membrane lining, its articular cartilage shock absorbing structure and function, subchondral bone micro fractures and bone marrow lesions. In addition, muscle and tendon attrition, nerve receptor alterations, and ligamentous damage of the incident joint such as the shoulder are common disabling correlates.
In the absence of any apparent tendency towards repair, the presence of one or more of the aforementioned complex chronic destructive joint changes commonly resulting in multiple challenging physical symptoms such as pain, stiffness, joint instability, muscle weakness, joint tenderness, and impaired mobility is rarely successfully attenuated or reversed [2, 3]. Moreover, at the shoulder joint, the condition, also termed glenohumeral osteoarthritis, may be accompanied by varying degrees of tendon damage or tendinopathy as well as extensive joint destruction due to remodelling of those bone surfaces and margins that lie adjacent to cartilage and interface with four key shoulder muscles, potentially affecting their humeral bone stabilizing and muscle reflex protective roles. As well, there may be varying degrees of: shoulder joint inflammation, tissue impingement, muscle fat infiltration and atrophy, muscle mass declines, active and passive movement limitations, losses of joint stability, joint deformity, joint kinematic alterations, diminished muscle endurance, functional challenges and adverse local and central reactive neural responses that contribute to the disease burden.
While generally deemed ‘untreatable’ other than by palliative medication approaches and surgery, research shows low intensity pulsed ultrasound [LIPUS], a non-thermal mode of biophysical energy with bone healing potential especially in the elderly [4, 5] may exert possible favorable regenerative mechanical and biochemical stimulatory effects on other osteoarthritis affected joint tissues, not only on bone cells [5-8]. In particular, they may deactivate those pathophysiological processes that arise from a dysregulation in the function of cytokines and growth factors, prostaglandins, cartilage matrix fragments, neuropeptides, reactive oxygen intermediates, proteolytic enzymes and protease inhibitors involved in fostering a cycle of cartilage, bone, ligaments, muscle and synovial impairments. Their application may successfully attenuate inflammatory responses and the degree of prevailing peripheral and central nervous system pain sensitization [3, 8, 9] and brain compensation responses in the face of perpetual shoulder dislocation [10]. As well, tendon-bone interfaces at the diseased shoulder joint that are essential for effective muscle modulation effects may be reinforced post LIPUS stimulation [11-13], as may possibly repair of articular cartilage and bone damage essential for reducing osteoarthritis disease severity [14-17].
Unsurprisingly, while still a realm of study that is not agreed upon by all and remains largely preclinical, LIPUS applications have been touted as being a possible intervention adjunct of high promise and clinical relevance both as a preventive as well as an auxiliary treatment measure with the potential to suppress degradation of articular chondrocytes even in the case of prevailing joint osteoarthritis [18]. Importantly in shoulder osteoarthritis, LIPUS may also impact tendon viability in the case of tears or pathological damage that does not heal at all effectively via intrinsic mechanisms or surgery alone [19-22], This is partly based on a tendon model that showed when compared to the control groups, those that received LIPUS treatments administered initially in the proliferation phase of the artificial tendon injury increased its tensile strength by approximately 30%, and its elasticity by approximately 53%, fibrillar appearance by 53%, and inflammation by 20% in a shorter time frame than anticipated even after only one week of stimulation [19].
These possible improvements and others [19-22] attributed to the impact of low but intermittent sound waves as they stimulate pathways of mechanical and structural influence at the cellular and molecular levels when applied to joint tissues such as cartilage or tendons or bone-tendon interfaces are potentially highly suitable for the treatment of vulnerable older adults with severe joint attrition and rotator tendon damage as opposed to high energy sound or shock wave applications advocated for some tendinopathies, but that may not be suitable for many frail or ill older adults to mitigate inflammation and cognitive impairments due to muscle atrophy that it may well prevent [23, 24] as well as influence favorable cell based microenvironment actions on and slowing of any excess or premature cell senescence and tendon inflammation [22, 25].
As noted by Sullivan et al. [26] these studies on LIPUS may be timely as there is a growing interest not only in preventive practices to counter osteoarthritis, but in employing potentially regenerative treatments aimed at alleviating its symptoms, averting excess damage, reinvigorating joint function and structure, enhancing quality of life, and potentially postponing invasive surgical interventions. In this regard, and backed up by at least four decades of research, it does appear safe to assume that when all issues are considered, applications of LIPUS if carefully construed can be used with confidence to address one or more features of disabling chronic shoulder osteoarthritis in older adults with less risk of harm and exacerbation of extensive shoulder osteoarthritis and chronic rotator cuff damage that could otherwise accrue from narcotics and excess or harmful exercises, or some forms of invasive injection or surgery.
Since many adults are at risk for shoulder osteoarthritis, but want to age ‘in place’, a search for some form of mitigation of this condition is increasingly supported as a desirable line of inquiry. This however, is especially challenging in the face of a widespread belief the disease is incurable, and its many overlapping disease factors where cause and effect are uncertain at best. Debilitating chronically disabling joint disease and its ramifications in general, and at the shoulder in particular if arm use is hampered, thus remain an immense public health concern, with few solutions [26], but with a high solution need in the face of global aging surges and its many arthritis related manifestations that arise largely in later life, but where independence is highly prized. Indeed, any modality that can safely offset its many adverse functional impacts, or promote healing of one or more of its probable disease features such as articular cartilage damage, subchondral bone micro fractures and pain, along with inflammation remains of high value in the face of its likely contribution to immense global health and socioeconomic costs, and suffering.
After researching this topic for more than 40 years it appears LIPUS can likely be applied to a joint deemed to be osteoarthritic with the expectation it may allay the disease progression or severity [29], while fostering articular cartilage chondro-protective or reparative effects as well as adjacent tendon tissue protective or anabolic effects. As a result, fewer medications including narcotics may be needed along with surgery [27, 28]. Its application may also reduce local pain due to synovial inflammation as well as possible central pain attributes and sensory sources and joint swelling [20- 32]. At the same time as providing a required cartilage mechanical stimulus to sustain needed to maintain cartilage mechanical and physiologic properties [29], skeletal muscle regeneration and the acceleration of soft tissue, cartilage, and bone healing processes may ensue in response to LIPUS applications [27, 33-35].
Hypotheses
LIPUS, if applied to offset or treat osteoarthritis, the most prevalent joint disease, may be able to: a) slow the rate of deterioration, while fostering articular cartilage repair bone and soft tissue healing, b) lower the magnitude of the suffering presently encountered worldwide by osteoarthritis sufferers especially if they want to age in place, c). provide a mechanism for fostering more direct drug delivery to cartilage cells or chondrocytes, or tendons, while positively affecting intracellular ion transport, cell signaling, and gene expression of adjacent support tissues.
Significance
In a search for promising disease modifying agents that are safe and cost-effective, and can possibly be employed at different stages of tissue engineering and regenerative strategies, it is possible LIPUS can be of help directly or as an adjunctive strategy [33, 34].
Aims
This brief specifically aimed to explore the data concerning the possible utility of LIPUS for treating shoulder or glenohumeral osteoarthritis directly and/or specifically, an area that truly has received almost no attention if compared to knee or hip osteoarthritis. While only a brief overview is provided, the topic was chosen for its rich preclinical support and the age grouping where few safe treatment options prevail.
Key questions
The key questions currently addressed are: 1) whether LIPUS is continuously being shown to produce uniform trends of significant impact to degraded joint structure or function; 2) whether the impacts observed support a role for LIPUS in efforts to foster better conservative as well as surgical shoulder osteoarthritis outcomes in cases requiring tendon repair or joint replacement.
Methods
To secure the desired topical research articles, the PUBMED, PubMed Central and Google Scholar databases housing most of the world’s available LIPUS based literature were selected. Acceptable publications were those that specifically focused on the impact of LIPUS on articular cartilage and tendon lesions, regardless of source, and only preclinical studies were examined as a basis for ascertaining a possible need for further research in this realm. No restriction was placed on the lab model employed, but outcomes examined had to reflect upon some relationship between LIPUS applications and chondrocyte function or cartilage composition or tenocyte impacts. Years specifically examined were January 1 2015 - Oct 15, 2025 using the key words articular cartilage, low intensity ultrasound [LIPUS], tendon damage and repair, shoulder osteoarthritis, older adults, rotator cuff lesions. All publications deemed eligible were screened, and accepted if deemed to fulfil the eligibility criteria. Background data on this topic were reviewed as well, and these items plus those from other sources such as CINAHL were included for clarity, as indicated. Excluded were studies including other modalities, studies on clinical samples, non-English studies and English abstracts or proposals. Articles on shock wave therapy were excluded as well.
Results
As with osteoarthritis in general, shoulder osteoarthritis is a highly disabling condition involving the whole joint and suffered by increasing numbers of young and older adults [3, 36, 37]. A relatively poorly studied osteoarthritis site, as opposed to that of the knee or hip joints, an array of medications and injections are commonly applied to provide temporary pain relief and improve function, but to no resounding structurally relevant reparative effect or advantage. At the same time, its causes other than injury are obscure, and the use of pain medication may provoke rather than protect against injury. Additionally, the multifactorial nature of the disease is complex and hard to unravel and renders the discovery and development of new drugs or biologics highly challenging [3].
Ultrasound, on the other hand, a physical modality used clinically for many years [38] and deliverable in various modes, including continuous versus pulsed ultrasound has been found to impact bone remodeling, as well cartilage repair. In this regard, externally applied LIPUS may offer a practical adjunctive form of intervention that may yield more favorable osteoarthritis related outcomes than not [39]. As per Cheng et al. [39] LIPUS applications may be found to afford means of curing osteoarthritis given the post LIPUS impacts observed on the expression of all tested genes, which was significantly increased except for that of metalloproteinase [a degrading enzyme], which was significantly decreased in the LIPUStreated osteoarthritis models group compared to the untreated osteoarthritis group. Moreover, LIPUS may affect the integrin- FAK-PI3K/Akt mechanochemical transduction pathway and alter chondrocyte matrix production by osteoarthritis chondrocytes favourably. Its use also appears promising as well for accelerating patient recovery after acute tendon and ligament injuries, as well as for muscle repair [34], and after surgical repair of bone-soft tissue junction injuries [40]. Moreover, LIPUS treatments appear capable of providing protection to ligament stem cells exposed to oxidative stresses as well as bone homeostasis [14] potentially favorable for osteoarthritis amelioration [15, 41]. LIPUS can also modulate pathways that govern cell death, as well as ameliorate the extent of any persistent damaging synovial inflammation responses found in osteoarthritis and can thereby potentially improve tendon histology and functional status in the face of tendon damage [42, 43].
Other data show LIPUS can impact cartilage cell and cartilage extracellular matrix metabolism that would otherwise lead to cartilage degeneration, synovitis and possible osteophyte formation [44, 45], while expediting tissue repair, nutrient delivery, and healing of damaged tissues and molecular signatures associated with downgrading chronic inflammation [46, 47]. As shown by Gaun et al. [44, 45] their pioneering work yielded verifiable biomechanical effects of LIPUS on living mice chondrocytes that implicated the potential to maintain cartilage homeostasis and enhance cartilageprotection in the face of joint damage quite decisively. Other data affirm LIPUS is effective in reducing synovial fibrosis [48] as well as in inhibiting inflammation, cartilage degeneration and disease progression [49] and can be shown to promote extracellular matrix synthesis and secretion, while reducing chondrocyte apoptosis or cell death [50].
Although lacking any widespread clinical based osteoarthritis study that could validate its intervention efficacy, these abovementioned cumulative results are still relevant because they are backed up by a host of carefully controlled lab studies and strong parallel mechanistic explanations that are observable and clinically relevant. They strongly imply LIPUS has significant mechanochemical transduction capacities and is a biophysical wave form that can be crafted in targeted ways to ‘help’ alter or reverse extracellular cartilage matrix production dysfunction as well as muscle atrophy [5, 51-53].
As such, it appears that some modes of LIPUS may be of profound benefit to older adults with shoulder joint damage who seek to live in the community. Their cumulative, timely, and time sensitive and emergent responses to applications applied over time at varying intensities do appear to also have the ability to foster cartilage repair as well as tendon repair [53, 54] and collagen type II expression [55, 56]. Hsieh et al. [55] who examined whether early intervention with LIPUS helps delay traumatically induced osteoarthritis progression in male Sprague-Dawley rats found that compared with the sham treatment, LIPUS significantly reduced Mankin scores, inflammatory cells and matrix metallopeptidase 13 expression in addition to increasing collagen type II expression.
Its usage is also shown to impact joint effusion, muscle regeneration, chondrocyte apoptosis, expression of anabolic versus catabolic cytokine levels and subchondral bone sclerosis, hallmarks of osteoarthritis pathology [57, 58]. It may have additional and highly desirable mechanistic and stimulatory influences on the healing of damaged shoulder tendons and ligaments, as well [40, 59] as important anti-inflammatory impacts [35] and cellular elements of cartilage [27]. In sum, regardless, of year of study, or the lab model, study methods and aims, degree of LIPUS exposure, and application mode, LIPUS applications tend to yield favorable outcomes in tissue cultures and diverse osteoarthritis models more often than not. In addition, several independent researchers have concluded these findings are based on distinctive observable LIPUS activated mechano chemical transduction and molecular signaling pathways that Favor joint homeostasis rather than any spurious effect and that may hold immense promise in the clinical realm in the future.
Discussion
Osteoarthritis a prevalent chronic multi-factorial degenerative joint disease characterized by: joint tissue inflammation, osteophyte or bone spur formation, subchondral bone fractures and attrition, capsular, and tendon sclerosis, muscle atrophy and fibrosis, and articular cartilage degradation is highly impairing and challenging to treat and often mars life quality and independence and wellbeing in many older adult populations quite significantly, especially at the shoulder joint [36, 37. 60, 61]. To intervene in the disease cycle and allay its progression and extent and offer some relief and promise of functionality, not achieved by most medication interventions, many ideas prevail, but in reality, still focus largely on drug, invasive injections and surgery associated interventions with less than optimal or desirable outcomes.
Ultrasound a form of biophysical energy widely used in medicine as both a diagnostic and therapeutic tool is a form of acoustic and mechanical energy that can be applied non thermally, to produce or harness a variety of favorable biological and metabolic effects in those tissues, cells, and pro and anti-inflammatory pathways implicated in osteoarthritis [62]. Indeed, many decades of study have shown that one can expect a favorable effect on joint tissues such bone and cartilage, implicated in osteoarthritis contexts and thereby do not align with the belief the disease is incurable [52]. It is indeed a mechanoregulatory technique that activated internal structures and physiology independent of thermal effects, and thereby safely delivers controlled mechanical stimuli to activate endogenous mechanotransduction pathways, such as ion channels, transmembrane proteins, and cytoskeleton-mediated signaling cascades that regulate critical cellular processes, such as proliferation, differentiation, and apoptosis [62].
As well, almost 20 years ago, Lee et al. [63] concluded LIPUS treatment had the potential to serve as efficient and cost-effective method for fostering cartilage tissue engineering attempts and others that could vastly improve the outlook for many, for example older adults with severe shoulder osteoarthritis who cannot undergo surgery. Using rabbit stem cells, these researchers found LIPUS increased: matrix formation; the expression of chondrogenic markers such as collagen type II, aggrecan, and Sox-9; and tissue inhibitor of metalloprotease-2 implicated in the fostering the integrity of cartilage matrix. In this respect, it appears that early intervention in this regard is likely to be more favorable than delayed intervention and will leave the individual better off biomechanically and functionally than if no LIPUS treatment is offered [49, 63, 64]. Its application may also be useful clinically for improving the quality of implants of live cells being tested for purposes of repairing small articular cartilage defects [65] and chondral histology [27], while preventing cartilage degradation [9] and the rate of disease development [49]. Stimulation may also reduce the emergent expression of matrix metalloprotease-13, a catabolic degradative over expressed protein found to cause cartilage destruction in osteoarthritis [27], while increasing type II collagen production [15], pain relief, function and life quality [66].
While models of osteoarthritis may not represent the actual processes of the human disease with a high degree of accuracy, and experimental set ups may not emulate the commonplace day to day cartilage influences of the osteoarthritic patient realistically, nor the clinical intervention practices that may exist, the available preclinical study results over the past 40 years or more clearly support the hypothesis that LIPUS can exert favorable biophysical influences on both normal chondrocytes, as well as those from osteoarthritic joint sources. These observed preclinical findings that appear to have been gleaned among differing models of osteoarthritis and a variety of laboratories with some degree of consistency, along with their carefully controlled designs in many cases, and well-established objective outcome tools presumably enhances the possible generalization of these favorable findings in the preclinical realm. Moreover, with additional research demonstrating reasonable evidence for a variety of plausible proposed biophysical mechanisms of action, along with some well-designed clinical studies that tend to show greater benefits of applications applied to osteoarthritic joints than not, the utility of this modality for fostering cartilage repair justifiably warrants more research.
One mechanism hypothesized to account for the repair of osteoarthritis cartilage observed by Loyola-Sanchez et al. [67] and others is its influence as a mechanotransducer [9, 29] that might influence cellular processes that impact cartilage structural features in a dose dependent manner as well as muscle strength that could be extrapolated to the bedside [68]. Another is that LIPUS stimulates chondrocyte proliferation and matrix production in human explants exposed to LIPUS [9, 29] via increases in aggrecan mRNA expression and proteoglycan synthesis by chondrocytes [69].
According to Whitney et al. [70] LIPUS, a form of mechanical stimulation exerts its influence via chondrocyte integrin receptors, MAPK/Erk and FAK, Src, p130Cas and CrkII pathways that can be targeted and may be poorly activated or suppressed in the presence of joint and possible nerve damage and neuropathic pain, amidst the absence of any related intervention attempts [39, 71-72] or delayed intervention applications [15] Applied in some way to impact early osteoarthritis positively on the other hand would undoubtedly be of immense value, especially in cases where tendon damage is considerable.
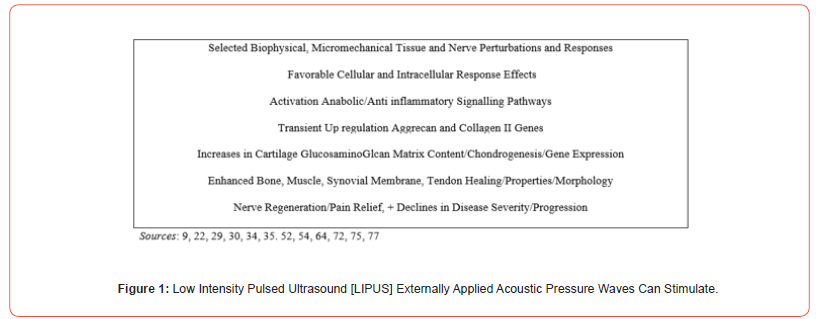
However, to advance these ideas and lab-based findings with any degree of confidence, research to strengthen the case for LIPUS is essential. Moreover, efforts to examine whether if used in conjunction with other cartilage promoting factors and strategically targeted dosages and frequencies of application and joint protection efforts will prove especially beneficial. LIPUS and its mechanical loading effect on joint tissues should also be explored from a biomechanical, structural, inflammatory, and mechanical perspective more intensely in the clinical setting and especially among older adults with various forms of osteoarthritis so as to both solidify the salient mechanisms underlying LIPUS applications in the context of various degrees of cartilage and soft tissue pathology as well as dose responses to varying acoustic energy modes. Examining the most optimal related time for purposes of attaining optimally beneficial effects, as well how best to deliver LIPUS to selected joint sites [73] including tendonbone interfaces will undoubtedly be helpful as well in this regard. In the interim we agree with the positive ideas of Zhang et al. [35] and outline some possible LIPUS features that appear to interact to yield observable potentially clinically non-destructive relevant tissue impacts that might be harnessed to minimize shoulder pain and dysfunction in at least some older osteoarthritis sufferers with risky health profiles. Here we assert:
Key Conclusions
Despite the obvious limitations of this current report, and its broad reliance on preclinical data we conclude externally applied LIPUS linked applications often used clinically to ameliorate osteoarthritis symptoms of pain has the potential to impact articular cartilage physiology and structure favorably as well as bone, muscle and the tendon healing attributes of its diverse pathologies, including osteoarthritis joint damage at the shoulder. Consequently, while osteoarthritis is generally deemed ‘untreatable’ other than by palliative medication approaches and surgery, research shows low intensity pulsed ultrasound, a non-thermal mode of biophysical stimulation has bone and cartilage healing potential that may not only reduce pain but may exert possible favorable mechanical and biochemical stimulatory effects on all osteoarthritis joint tissues, including muscle, tendon, and nerve cells and tissues.
Building on an immense research foundation spanning four decades, we further conclude researchers can expect one or more promising functional results or results that exceed current expectations and are not attributable to placebo if the damaged tissues are subjected to carefully targeted and tailored applications. This may safely and effectively assist those older adults who may suffer severely, but are not eligible for surgery. In this regard, we further conclude early rather than delayed interventions are likely to prove viable as far as optimizing osteoarthritis cartilage, muscle, bone and tendon repair in the older adult with severe shoulder joint damage. A better understanding of the impacts of LIPUS mechanical stimulation on gene regulatory mechanisms in general and especially in human tissue substrates in health as well as disease situations may also prove valuable and open new doors of clinical insight and opportunity [70-79].
Indeed, even if preclinical cellular or laboratory based artificially developed tissue lesions or animal models of arthritis cannot be equated with or extrapolated to any in vivo situation with any degree of certainty, noteworthy LIPUS impacts reported in this regard that stem from an increasing number of well-controlled and designed preclinical studies and isolated clinical studies are promising in multiple spheres including bone and wound healing and inflammation reduction [78-80]. Additionally, it is possible the many favorable preclinical underpinnings observed to date regarding LIPUS applications to joint damage may be further enhanced in the face of more advanced technical instrumentation and the concomitant application of biomechanical, neurosensory, serum assays and kinematic measures. Moreover, while one cannot exclude publication bias as the reason for the trends demonstrated to date, and the fact negative studies are less well represented in the literature in general, most lab-based studies where the placebo effect is unlikely yield one or more apparent reparative post stimulation benefits. While clinical studies may be underpowered and thus fail to corroborate the many post LIPUS regenerative indications observed across time, most are poorly controlled and/or fail to examine salient potential impacts such as changes at the cartilage bone interface, thus failing to demonstrate a possible measureable clinically relevant impact. Yet even here, diverse data from the clinic continue to support the potential value of further examining the efficacy of low pulse clinical ultrasound for ameliorating osteoarthritis symptoms, regardless of target tissue stimulated, and where its optimal mode of application and frequency and duration that need to be carefully selected, crafted and tailored can be tested rigorously.
In particular, it appears important to go beyond cross-sectional inferences and secure more interest in examining controlled longitudinal studies formulated with possible support from artificial intelligence [AI] diagnostics plus state-of-the-art objective measures that can capture efficacy as well as mechanistic data when applied to various degrees of shoulder osteoarthritis in the older adult. Currently a relatively untapped area of clinical research and practice, more rapid much needed advancements may ensue by applying the ideas of Miller et al. [74] as regards matching the frequency of the driving force of LIPUS to that of the chondrocyte system’s natural frequency of vibration so as to foster more possible tissue healing and valuable intracellular cell pathway signaling responses than those achieved in the face of random LIPUS applications. The frequencies selected should also match the target cell mass and estimated degree of intracellular stiffness, as well as the mechanical properties of the surrounding medium and can perhaps be supported and implemented here if we consider the ability of AI diagnostics to delineate these attributes and others. In sum, we conclude translating and refining the promising past and emergent LIPUS-shoulder lesion data and uncovering more insights into its explanatory and response mechanisms sooner rather than later will yield enormous societal as well as individual health impacts plus multiple disease insights and advances in reparative as well as clinical medicine.
Closing Remarks
As per Qin et al [76], we concur that until more research is forthcoming, it appears a large reference frame supports the use of LIPUS applications to mitigate multiple forms of joint damage such as those that emerge at the shoulder in many older adults that appear progressive and irreversible. Applied at all disease stages and regardless of disease extent and severity, the practitioner can expect LIPUS strategies to safely reduce pain and promote favorable mechanochemical induced cartilage and joint tissue healing and regenerative processes as well as slow its disabling progressive impacts on day-to-day function and independence, even in the face of surgery.
Acknowledgement
None.
Conflict of Interest
No conflict of interest.
References
- Allen Kelli D, LM Thoma, YM Golightly (2022) Epidemiology of osteoarthritis. Osteoarthritis and Cartilage 30(2): 184-195.
- Jing Zhou, Eryu Ning, Lingfeng Lu, Huili Zhang, Xing Yang, et al. (2024) Effectiveness of low-intensity pulsed ultrasound on osteoarthritis: molecular mechanism and tissue engineering. Frontiers in Medicine 11: 1292473.
- Heike A Wieland, Martin Michaelis, Bernhard J Kirschbaum, Karl A Rudolphi (2005) Osteoarthritis-an untreatable disease? Nature reviews Drug Discovery 4(4): 331-344.
- Harrison Andrew, Volker Alt (2021) Low-intensity pulsed ultrasound LIPUS) for stimulation of bone healing-A narrative review. Injury 52: S91-S96.
- Xiaofei Li, Yueli Sun, Zhilun Zhou, Dongye Zhang, Jian Jiao, et al. (2019) Mitigation of articular cartilage degeneration and subchondral bone sclerosis in osteoarthritis progression using low-intensity ultrasound stimulation. Ultrasound in Medicine & Biology 45(1): 148-159.
- Jumpei Sekino, Mayu Nagao, Shunichiro Kato, Mayu Sakai, Kimiko Abe, et al. (2018) Low-intensity pulsed ultrasound induces cartilage matrix synthesis and reduced MMP13 expression in chondrocytes. Biochemical and Biophysical Research Communications 506(1): 290-297.
- Tatsuya Shimizu, Naomasa Fujita, Kiyomi Tsuji-Tamura, Yoshimasa Kitagawa, Toshiaki Fujisawa, et al. (2021) Osteocytes as main responders to low-intensity pulsed ultrasound treatment during fracture healing. Scientific Reports 11(1): 10298.
- Stephanie Petterson, Kevin Plancher, Dominic Klyve, David Draper, Ralph Ortiz (2020) Low-intensity continuous ultrasound for the symptomatic treatment of upper shoulder and neck pain: a randomized, double-blind placebo-controlled clinical trial. Journal of Pain Research 13: 1277-1287.
- Uddin Sardar MZ, David E. Komatsu (2020) Therapeutic potential low-intensity pulsed ultrasound for osteoarthritis: pre-clinical and clinical perspectives. Ultrasound in Medicine & Biology 46(4): 909-920.
- Hitoshi Shitara, Kenji Takagishi, Daisuke Shimoyama, Tsuyoshi Ichinose, Atsushi Yamamoto, et al. (2014) Compensatory change of brain in recurrent anterior shoulder dislocation-fMRI study. Journal of Shoulder and Elbow Surgery 23(5): 601.
- Ayoola Ibifubara Aiyegbusi, Francis Ikechukwu O Duru, Sunday Rufus A Akinbo (2012) The morphology of the healing tendon: a comparison of the effects of intrasound therapy and therapeutic pulsed ultrasound. Connective Tissue Research 53(6): 478-484.
- Issei Nagura, Takeshi Kokubu, Yutaka Mifune, Atsuyuki Inui, Yoshifumi Harada, et al. (2014) The effect of low-intensity pulsed ultrasound for tenogenesis of human rotator cuff cells. Journal of Shoulder and Elbow Surgery 23(5): 601.
- Zihan Xu, Shengcan Li, Liyang Wan, Jianzhong Hu, Hongbin Lu, et al. (2023) Role of low‐intensity pulsed ultrasound in regulating macrophage polarization to accelerate tendon-bone interface repair. Journal of Orthopaedic Research® 41(5): 919-929.
- Tang Li, et al. (2025) LIPUS Protects PDLSCs from oxidative damage and promotes alveolar bone regeneration via FOXO1. Oral Diseases.
- Xia Peng, et al. (2015) Low‐intensity pulsed ultrasound treatment at an early osteoarthritis stage protects rabbit cartilage from damage via the integrin/focal adhesion kinase/mitogen‐activated protein kinase signaling pathway. Journal of Ultrasound in Medicine 34(11): 1991-1999.
- Massari Leo, et al. (2019) Biophysical stimulation of bone and cartilage: state of the art and future perspectives. International Orthopaedics 43(3): 539-551.
- Xiao Han, et al. (2023) LIPUS accelerates bone regeneration via HDAC6-mediated Ciliogenesis. Biochemical and Biophysical Research Communications 641: 34-41.
- Iwabuchi Yasunori, et al. (2014) Effects of low-intensity pulsed ultrasound on the expression of cyclooxygenase-2 in mandibular condylar chondrocytes. J Oral Facial Pain Headache 28(3): 261-8.
- Kurtulmuş Tuhan, et al. (2024) Effect of the low-intensity pulsed ultrasound therapy on healing of Achilles tendinopathy in a rat model. Acta Orthopaedica et Traumatologica Turcica 58(2): 102.
- Chen Junjie, et al. (2023) A review of the role of tendon stem cells in tendon-bone regeneration. Medical Science Monitor: International Medical Journal of Experimental and Clinical Research 29: e940805-1.
- Desmeules François, et al. (2015) The efficacy of therapeutic ultrasound for rotator cuff tendinopathy: A systematic review and meta-analysis. Physical Therapy in Sport 16(3): 276-284.
- Li Shengcan, et al. (2021) Acceleration of bone-tendon interface healing by low-intensity pulsed ultrasound is mediated by macrophages. Physical Therapy 101(7): pzab055.
- Wang Wanzhao, et al. (2023) Low-intensity pulsed ultrasound mitigates cognitive impairment by inhibiting muscle atrophy in hindlimb unloaded mice. The Journal of the Acoustical Society of America 154(3): 1427-1438.
- Yang Xuebing, et al. (2022) Integrated application of low-intensity pulsed ultrasound in diagnosis and treatment of atrophied skeletal muscle induced in tail-suspended rats. International Journal of Molecular Sciences 23(18): 10369.
- Han W, Guan M, Liao B, Han X, Li K, et al. (2025) Low-intensity pulsed ultrasound inhibits chondrocyte senescence by inhibiting PI3K/AKT/mTOR signaling. Brazilian Journal of Medical and Biological Research 58: e14408.
- Sullivan Erin, et al. (2025) A novel treatment for combined adhesive capsulitis and glenohumeral osteoarthritis–case study: RELIEF: ®: treatment. Orthopaedic Nursing 44(3): 167-174.
- Rothenberg, Joshua B, et al. (2017) The role of low-intensity pulsed ultrasound on cartilage healing in knee osteoarthritis: a review. PM&R 9(12): 1268-1277.
- Li Xinhe, et al. (2025) Ultrasound-responsive piezoelectric analgesic microspheres alleviate osteoarthritis pain. Journal of Controlled Release 385: 114049.
- Lee Wonsae, et al. (2024) Daily low-intensity pulsed ultrasound stimulation mitigates joint degradation and pain in a post-traumatic osteoarthritis rat model. Journal of Orthopaedic Translation 44: 9-18.
- Zhao Long, et al. (2025) Efficacy of focused low intensity pulsed ultrasound in reducing lower-extremity swelling and pain after total knee arthroplasty: a randomized study. International Orthopaedics: 1-9.
- Chung JI, et al. (2012) Anti-inflammatory effect of low intensity ultrasound (LIUS) on complete Freund's adjuvant-induced arthritis synovium. Osteoarthritis and Cartilage 20(4): 314-322.
- Smallcomb Molly, et al. (2022) Therapeutic ultrasound and shockwave therapy for tendinopathy: a narrative review. American Journal of Physical Medicine & Rehabilitation 101(8): 801-807.
- Qin Haocheng, et al. (2023) Low-intensity pulsed ultrasound promotes skeletal muscle regeneration via modulating the inflammatory immune microenvironment. International Journal of Biological Sciences 19(4): 1123-1145.
- Zhang Bin, et al. (2020) SQSTM1-dependent autophagic degradation of PKM2 inhibits the production of mature IL1B/IL-1β and contributes to LIPUS-mediated anti-inflammatory effect. Autophagy 16(7): 1262-1278.
- Stanborough Rupert O, Joseph M Bestic, Jeffrey J Peterson (2022) Shoulder osteoarthritis. Radiologic Clinics of North America 60(4): 593-603.
- Vocelle Amber R, Garrett Weidig, Tamara R Bush (2022) Shoulder structure and function: The impact of osteoarthritis and rehabilitation strategies. Journal of Hand Therapy 35(3): 377-387.
- Guan Mengtong, et al. (2025) Research progress of osteoarthritis treatment by low intensity pulsed ultrasound. Smart Medicine 4(2): e70003.
- Cheng Kai, et al. (2014) Effects of low-intensity pulsed ultrasound on integrin-FAK-PI3K/Akt mechanochemical transduction in rabbit osteoarthritis chondrocytes. Ultrasound in Medicine & Biology 40(7): 1609-1618.
- Lai Wilson C, et al. (2021) Low-intensity pulsed ultrasound augments tendon, ligament, and bone-soft tissue healing in preclinical animal models: a systematic review. Arthroscopy: The Journal of Arthroscopic & Related Surgery 37(7): 2318-2333.
- Fujita Mutsumi, et al. (2019) Protective effects of low-intensity pulsed ultrasound on mandibular condylar cartilage exposed to mechanical overloading. Ultrasound in Medicine & Biology 45(4): 944-953.
- Zhang Bin, et al. (2024) Research trends and perspective of low-intensity pulsed ultrasound in orthopedic rehabilitation treatment based on Web of Science: A bibliometric analysis. Journal of Back and Musculoskeletal Rehabilitation 37(5): 1189-1203.
- İnceoğlu Alperen, et al. (2021) Effects of low-density pulsed ultrasound treatment on transforming growth factor-beta, collagen level, histology, biomechanics, and function in repaired rat tendons. Turkish Journal of Physical Medicine and Rehabilitation 67(2): 167-174.
- Guan Mengtong, et al. (2020) Low‐intensity pulsed ultrasound inhibits VEGFA expression in chondrocytes and protects against cartilage degeneration in experimental osteoarthritis. FEBS Open Bio 10(3): 434-443.
- Guan Mengtong, et al. (2025) LIPUS promotes calcium oscillation and enhances calcium dependent autophagy of chondrocytes to alleviate osteoarthritis. Advanced Science 12(16): 2413930.
- Li Xueping, et al. (2013) The effects of low-intensity pulsed ultrasound and nanomagnet applications on the expressions of MMP-13 and MAPKs in rabbit knee osteoarthritis. Journal of Nanoscience and Nanotechnology 13(1): 722-727.
- Liu Wencai, et al. (2025) Inflammatory cell interactions in the rotator cuff microenvironment: insights from single‐cell sequencing. International Journal of Genomics 2025(1): 6175946.
- Liao Qing, Jun Chen, Gang Liu (2025) Low intensity pulsed ultrasound alleviates synovial fibrosis in osteoarthritis via the PI3K/AKT pathway. Scientific Reports 15: 14807.
- Pan Chunran, et al. (2024) Low-intensity pulsed ultrasound delays the progression of osteoarthritis by regulating the YAP–RIPK1–NF-κB axis and influencing autophagy. Journal of Translational Medicine 22(1): 286.
- Ding Weizhong, Dengli Du, Shirong Chen (2020) LIPUS promotes synthesis and secretion of extracellular matrix and reduces cell apoptosis in human osteoarthritis through upregulation of SOX9 expression. International journal of clinical and experimental pathology 13(4): 810-817.
- Sun Lijun, et al. (2021) Molecular and metabolic mechanism of low-intensity pulsed ultrasound improving muscle atrophy in hindlimb unloading rats. International Journal of Molecular Sciences 22(22): 12112.
- Nishida T, et al. (2017) Low-intensity pulsed ultrasound (LIPUS) treatment of cultured chondrocytes stimulates production of CCN family protein 2 (CCN2), a protein involved in the regeneration of articular cartilage: mechanism underlying this stimulation. Osteoarthritis and Cartilage 25(5): 759-769.
- Yi Weiwei, et al. (2021) LIPUS inhibits inflammation and catabolism through the NF‐κB pathway in human degenerative nucleus pulposus cells. Journal of Orthopaedic Surgery and Research 16(1): 619.
- Choi Byung Hyune, et al. (2006) Low‐intensity ultrasound stimulates the viability and matrix gene expression of human articular chondrocytes in alginate bead culture. Journal of Biomedical Materials Research Part A 79(4): 858-864.
- Hsieh Yueh-Ling, Han-Yu Chen, Chen-Chia Yang (2018) Early intervention with therapeutic low-intensity pulsed ultrasound in halting the progression of post-traumatic osteoarthritis in a rat model. Ultrasound in Medicine & Biology 44(12): 2637-2645.
- He Dong, et al. (2021) Low-intensity pulsed ultrasound promotes aggrecan expression via ZNT-9 in temporomandibular joint chondrocytes. Gene 768: 145318.
- Jia Lang, et al. (2016) Focused low-intensity pulsed ultrasound affects extracellular matrix degradation via decreasing chondrocyte apoptosis and inflammatory mediators in a surgically induced osteoarthritic rabbit model. Ultrasound in Medicine & Biology 42(1): 208-219.
- Li Xueke, et al. (2023) Recent advances in the molecular mechanisms of low-intensity pulsed ultrasound against inflammation. Journal of Molecular Medicine 101(4): 361-374.
- Aliabouzar Mitra, Lijie Grace Zhang, Kausik Sarkar (2016) Lipid coated microbubbles and low intensity pulsed ultrasound enhance chondrogenesis of human mesenchymal stem cells in 3D printed scaffolds. Scientific Reports 6(1): 37728.
- Sang Fei, et al. (2021) Low-intensity pulsed ultrasound alleviates osteoarthritis condition through focal adhesion kinase–mediated chondrocyte proliferation and differentiation. Cartilage 13(2_suppl): 196S-203S.
- Zhou Hang-yu, et al. (2019) Low-intensity pulsed ultrasound repair in mandibular condylar cartilage injury rabbit model. Archives of Oral Biology 104: 60-66.
- Lei Lingling, et al. (2025) Mechanoregulation of cell fate by low-intensity pulsed ultrasound: Mechanisms and advances in regenerative medicine. BIO Integration 6(1): 1-18.
- Lee Hyun Jung, et al. (2006) Low‐intensity ultrasound stimulation enhances chondrogenic differentiation in alginate culture of mesenchymal stem cells. Artificial organs 30(9): 707-715.
- Naito Kiyohito, et al. (2010) Low‐intensity pulsed ultrasound (LIPUS) increases the articular cartilage type II collagen in a rat osteoarthritis model. Journal of Orthopaedic Research 28(3): 361-369.
- Nishikori T, et al. (2002) Effects of low‐intensity pulsed ultrasound on proliferation and chondroitin sulfate synthesis of cultured chondrocytes embedded in Atelocollagen® gel. Journal of Biomedical Materials Researc 59(2): 201-206.
- Jo Nam-Gyu, et al. (2022) The efficacy of low-intensity pulsed ultrasound on articular cartilage and clinical evaluations in patients with knee osteoarthritis. Journal of Back and Musculoskeletal Rehabilitation 35(6): 1381-1389.
- Loyola-Sánchez, Adalberto, et al. (2012) Effect of low-intensity pulsed ultrasound on the cartilage repair in people with mild to moderate knee osteoarthritis: a double-blinded, randomized, placebo-controlled pilot study. Archives of Physical Medicine and Rehabilitation 93(1): 35-42.
- Draper David O, et al. (2018) Effect of low-intensity long-duration ultrasound on the symptomatic relief of knee osteoarthritis: a randomized, placebo-controlled double-blind study. Journal of Orthopaedic Surgery and Research 13(1): 257.
- Parvizi Javad, et al. (1999) Low‐intensity ultrasound stimulates proteoglycan synthesis in rat chondrocytes by increasing aggrecan gene expression. Journal of Orthopaedic Research 17(4): 488-494.
- Whitney Nicholas P, et al. (2012) Integrin-mediated mechanotransduction pathway of low-intensity continuous ultrasound in human chondrocytes. Ultrasound in Medicine & Biology 38(10): 1734-1743.
- Wu Sha, et al. (2024) LIPUS regulates the progression of knee osteoarthritis in mice through primary cilia-mediated TRPV4 channels. Apoptosis 29(5-6): 785-798.
- Acheta Jenica, et al. (2022) Therapeutic low-intensity ultrasound for peripheral nerve regeneration–a schwann cell perspective. Frontiers in Cellular Neuroscience 15: 812588.
- White D, et al. (2007) Can ultrasound propagate in the joint space of a human knee? Ultrasound in Medicine & Biology 33(7): 1104-1111.
- Miller April D, et al. (2017) Frequency sensitive mechanism in low-intensity ultrasound enhanced bioeffects. PLoS One 12(8): e0181717.
- Fu Shijie, et al. (2023) External stimulation: a potential therapeutic strategy for tendon-bone healing. Frontiers in Bioengineering and Biotechnology 11: 1150290.
- Qin Haocheng, et al. (2022) The therapeutic effects of low-intensity pulsed ultrasound in musculoskeletal soft tissue injuries: focusing on the molecular mechanism. Frontiers in Bioengineering and Biotechnology 10: 1080430.
- Duan Huimin, et al. (2024) Low-intensity pulsed ultrasound (LIPUS) promotes skeletal muscle regeneration by regulating PGC-1α/AMPK/GLUT4 pathways in satellite cells/myoblasts. Cellular Signalling 117: 111097.
- Liang Wenxin, et al. (2024) Low-intensity pulsed ultrasound: a physical stimulus with immunomodulatory and anti-inflammatory potential. Annals of Biomedical Engineering 52(8): 1955-1981.
- Manferdini Cristina, et al. (2025) Ultrasound as new perspective system for modulation of joint osteoarthritic tissues. Osteoarthritis and Cartilage 33: S354-S355.
- Khanna Anil, et al. (2009) The effects of LIPUS on soft-tissue healing: a review of literature. British Medical Bulletin 89(1): 169-182.






